“The enemy of my enemy is my friend” – Proverb
Over years of evolution, our immune system successfully dealt with a variety of foreign invaders such as viruses, bacteria, fungi, and uni- and multi-cellular parasites. Starting 1900s, doctors and scientists started discovering a faulty immune system (mainly T and B cells) in patients, attacking their tissues – thus named the process – autoimmunity. Of course, some mechanisms prevent this cellular misunderstanding within our body, but we can get autoimmune diseases if they fail. This impaired immune regulation projects itself in many forms, including but not limited to, system lupus erythematosus (SLE), multiple sclerosis (MS), type I diabetes, celiac disease (CeD), inflammatory bowel disease, rheumatoid arthritis, and Hashimoto’s thyroiditis. About 3% of the US population currently suffers from autoimmunity and requires life-long therapy, causing an enormous burden for the healthcare system. Studying immune regulation to overcome autoimmunity has been a priority of scientists for decades now.
Animal models are one of the approaches for studying immune regulation during autoimmune diseases. For instance, we can investigate MS (a disease in which the myelin covering membranes of nerve cells in the spinal cord and brain are damaged) in the experimental autoimmune encephalitis (EAE) mice model. This model consists of a cytotoxic T cell subset with regulatory function (Ly49+CD8+T cells) that can suppress pathogenic CD4+ T cells and ameliorate EAE.
Envious of the mice’s luck, we question, do humans have a similar CD8+ regulatory T cells subset?
This and many other related questions came to the focus of Li and colleagues in their recent study.
The authors seem to have not missed a class on evolution, and hence knew that “nothing in biology makes sense except in the light of evolution”. Therefore, in pursuit of human CD8+ regulatory T cells, they selected a cell subset that expresses the evolutionary counterpart of the mouse Ly49 family receptors (this molecule confirmed as a hallmark of CD8+ regulatory T cells in mice), called the killer cell immunoglobulin-like receptors (KIRs).
Next, the authors measured the frequency of KIR+CD8+ T cells in patients with 1. autoimmune diseases like MS, SLE, and CeD, as well as 2. infectious diseases like COVID-19 and flu and compared with healthy individuals. They found that KIR+CD8+ T cells were significantly increased in the blood and affected tissues of patients with both autoimmune and infectious diseases. Interestingly, the levels of KIR+CD8+ T cells correlated with disease severity, vasculitis, and embolism in COVID-19 patients. At the same time, the authors did not find such a correlation with another well-known regulatory cell subset – CD4+ regulatory T cells or just Tregs (but don’t confuse them with T. rex).
To investigate if KIR+CD8+ T cells are the functional counterpart of mouse Ly49+CD8+ T cells and can deal with pathogenic CD4+ T cells, the authors chose to study CeD. CeD is an autoimmune disorder of the small intestine induced by gluten in genetically predisposed people. The principal role in the pathogenesis of CeD is played by gliadin specific CD4+ T cells. Thus, it is a perfect target for human KIR+CD8+ T cells to show if they can cope with this as their mice counterparts with myelin specific CD4+ T cells during EAE. KIR+CD8+ T cells accomplish the mission, specifically by eliminating pathogenic CD4+ T cells from the leukocyte population of CeD patients in vitro. Moreover, they used a similar mechanism to their mouse friends – inducing apoptosis of gliadin-specific CD4+ T cells. Further RNA sequencing analysis showed that human KIR+CD8+ T cells and mice Ly49+CD8+ T cells share many common features, suggesting their phenotypic and functional equivalence.
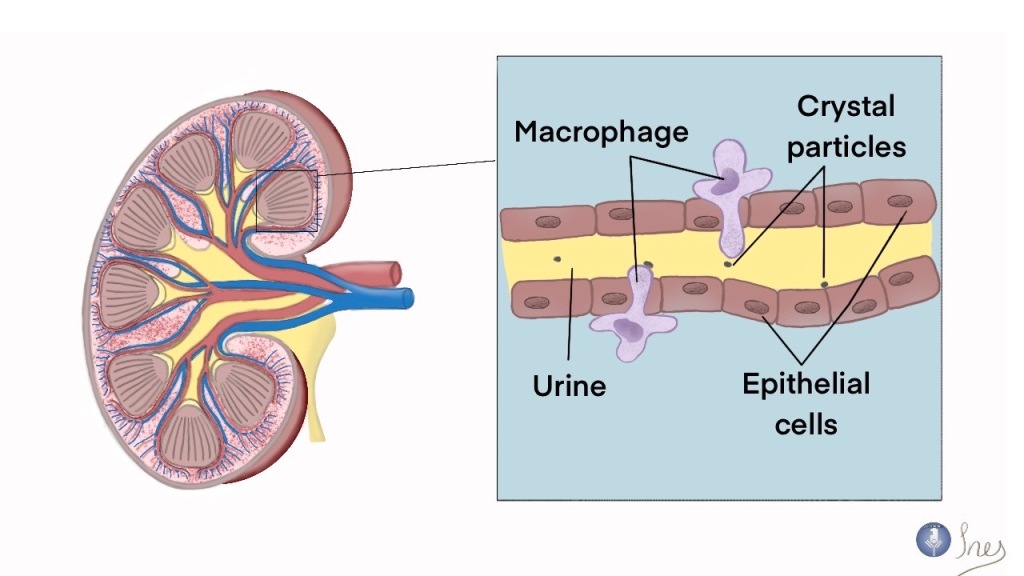
Finally, Li and colleagues investigated the role of KIR+CD8+ T cells in viral infections. They engineered Ly49+CD8+ T cells depleted mice and infected them with lymphocytic choriomeningitis virus (LCMV) or influenza virus. Such mice showed comparable viral clearance with the infected controls. However, Ly49+CD8+ T cells deficient mice developed autoimmune disease characterized by an increased number of CD4+ T follicular helper (TFH) (helping B cells to produce neutralizing antibodies) cells, glomerular nephritis, and pathogenic antibodies deposition in the kidney 30 days after LCMV infection. Similarly, the influenza-infected mice were observed with a peribronchial and interstitial accumulation of inflammatory cells with tissue fibrosis in the lung 60 days after infection. The authors concluded that regulatory CD8+ T cells are not involved in the immune response against pathogens directly but appear to control potential autoimmunity after viral infection.
So, now, having a new member in the human “regulatory club”, we can extend the general picture of pathogenic immune responses control (see the scheme). For instance, during the immune response, activated CD4+ T cells help CD8+ T cells in the killing of virus-infected cells of the host. At germinal centers of lymph nodes, activated CD4+ TFH cells help B cells to produce neutralizing antibodies. Before, we knew that FOXP3+CD4+ Tregs (the more official name of Tregs) could control these processes by preventing autoimmunity and tissue damage. Li et al. showed that human KIR+CD8+ T cells could eliminate activated pathogenic CD4+ T cells and CD4+ TFH cells and maintain peripheral tolerance in another than Treg form, likely complementing their function.
Despite that newly described CD8+ T regulatory cells in humans shed light on our understanding of the relationship between autoimmunity and infectious diseases and create space for therapeutic approaches, there are still many questions that we have to answer. Let’s stay tuned for this intriguing story.
Source:

Article author: Taras Baranovskyi. Taras is a medical doctor at Immunotherapy Clinic in Kyiv, Ukraine. His research is focused on developing new approaches for overcoming the antimicrobial resistance of Klebsiella pneumoniae. Also, Taras is a part of a team which spreads knowledge of immunology through the ‘Cup of Immunology’ project.
Editor: Sutonuka Bhar. Sutonuka is a scientist working on biotherapeutics development. She achieved her doctoral degree from University of Florida where her work focused on host immune responses against viruses and bacterial membrane vesicles.
Check out Antibuddies’ blog post “The Battle of the Ts: Regulatory CD8+ T cells suppress autoimmunity associated CD4+ T cells”.

Leave a comment